Calcified root canals, as the name suggests are calcium deposits in the root canals of a tooth. They are a challenge to dentists and endodontists. Root canals are usually hollow or have pulp tissue in them. There are various reasons as to why calcified root canals occur. In this article, we are going to see how and why calcified root canals occur.
What are the causes of calcified root canals?
The different reasons why calcified root canals occur include:
- Age
- Prolonged trauma
- Chronic Infection
- Tooth decay
- Coronal gum recession
- Improper dental fillings or crowns
How to deal with calcified root canals?
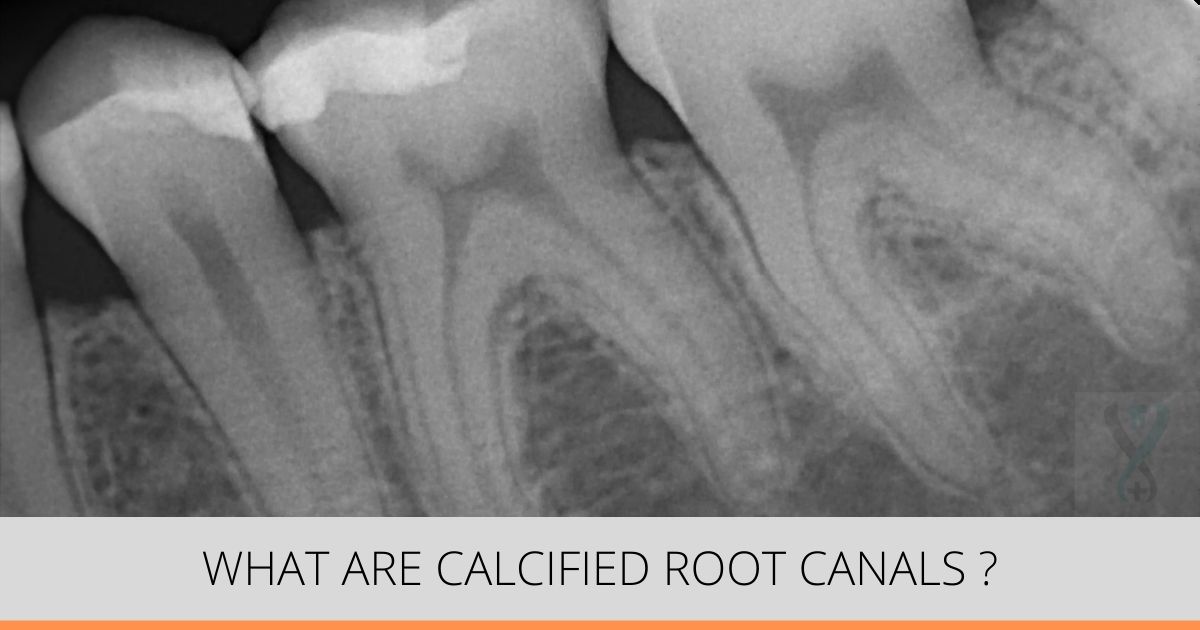
Usually, the calcification begins from the coronal portion (or the topmost) of the root canal. The apical or the bottom tip of the root canal is generally less calcified.
The coronal region of the root canal is the first to calcify due to a variety of reasons. The pulp calcification is seen as masses of calcified tissue close to the pulp chamber and roots of the tooth. These calcifications can occur as discrete pulp stones, pulp nodules or diffused calcifications.
Calcified canals can make it difficult for instruments to reach into the root canals for cleaning because the coronal or the top location makes it difficult for any instrument to pass to the tip of the root canal. That is, the calcified root canal is too narrow for instruments to be used for non-surgical root canal treatment. So it normally takes two sittings for the root canal treatment if the person has calcified or blocked root canal. This is because the block has to be softened prior to doing the actual root canal treatment. In partially calcified canals chelating agents like EDTA are used to clear up some of the calcified regions.